Numb chin syndrome as the first manifestation of an advanced metastatic cancer
Article information
Dear Editor,
Numb chin syndrome refers to reduced or absent sensation in an area over the chin and lower lip within the distribution of the mental or inferior alveolar nerves [1]. The term “numb chin syndrome” was first used in case reports of five patients who presented numbness on chin due to various malignancies in 1963 [2].
The chin numbness can be overlooked by patients and even clinicians because this is a pure sensory neuropathy limited to a relatively small area. However, numb chin syndrome can be associated with some fatal diseases. It may be the first and only manifestation of an advanced metastatic cancer [1,3–6]. In this case, the diagnosis will be severely delayed unless the clinician has suspicion and performs a thorough investigation. Here, we report a patient presenting with numb chin syndrome as the first manifestation of systemic malignancies.
An 80 years-old male presented with left chin numbness, which he noticed 3 weeks ago. The symptom was initially numbness accompanied by throbbing pain in the left lower chin, but the pain improved afterwards and the hypoesthesia continued. He had no past medical history and there was no family history. Neurological examination revealed decreased sensation to touch and pain in mandibular division of trigeminal cranial nerve below the lower lip on left side with sparing of motor function of the trigeminal nerve. All other cranial nerves were intact, and other central nervous system examinations and the peripheral nervous examination were normal.
Laboratory tests including serum tumor markers were not remarkable. We tested the blink reflex and confirmed the trigeminal nerve damage on the left side. A facial bone magnetic resonance imaging (MRI) showed soft tissue masses involving the ramus of both mandible, clivus, dorsum sella, and left maxilla, suggesting multiple bone metastases of cancer (Figure 1A, B). A whole-body 18 fluorine-fluorodeoxyglucose positron emission tomography study combined with computed tomography (18F-FDG PET/CT) demonstrated multiple hypermetabolic bone lesions throughout most of the body including skull base, facial bones, spines, and four limbs, but there were no predominant lesions suggestive of primary cancer (Figure 1C, D). Additional tests including blood test, chest and abdomen CT were performed to find the primary cancer, but no significant findings were found. We consulted with the oncologist and the patient decided to continue oncology treatment through outpatient clinic and was discharged.
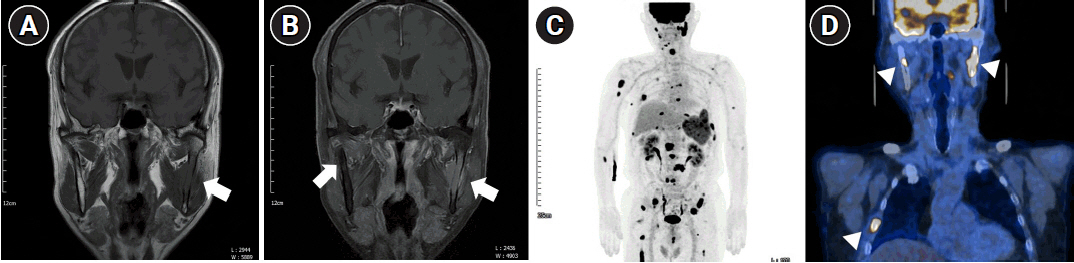
Facial bone magnetic resonance imaging (MRI) and whole-body 18 fluorine-fluorodeoxyglucose positron emission tomography study combined with computed tomography (18F-FDG PET/CT) study of a patient with numb chin syndrome. T1-weighted (A) and gadolinium enhanced T1-weighted (B) facial bone MRI demonstrate soft tissue mass involving ramus of both mandible (arrows). A whole-body 18F-FDG PET/CT (C, D) demonstrates multiple hypermetabolic bone lesions including skull base, both mandible, ribs (arrowheads), spines, and all four extremities.
Numb chin syndrome is a condition that can be easily overlooked because it is relatively mild symptom that does not significantly affect daily life. It is usually caused by dental problems including odontogenic-dental abscess or tumors, osteomyelitis of the mandible, trauma, and dental procedures. It also can be associated with systemic infectious or inflammatory conditions, including Lyme disease, human immunodeficiency virus infection, sarcoidosis, vasculitis or giant-cell arteritis. Several medications like bisphosphonate and mefloquine have been reported to cause osteonecrosis of mandible, resulting in numb chin syndrome [7].
Meanwhile, one of the most important causes that should not be missed, even if it is rare, is systemic malignancy. According to one retrospective study, less than 1% of cancers invade the mandible [8]. However, among patients with numb chin syndrome caused by metastatic cancer, it has been reported that it is the first manifestation in up to 47% of cases [1].
In a systematic review of 136 patients from 16 studies on numb chin syndrome associated with malignancies, leukemia (5.1%), prostate cancer (6.6%), lymphoma (20.5%) and breast cancer(40.4%) were most frequent in that order [9].
The pathophysiology of this syndrome in cases of systemic malignancy is mainly thought to be direct nerve compression or cancer invasion into the nerves, bone marrow, or bone. In addition, leptomeningeal metastases and paraneoplastic processes are also assumed to be possible mechanisms associated with distant neoplasms [1].
The prognosis for cancer-related numb chin syndrome is generally considered poor. When numb chin syndrome occurred in patients who had already been diagnosed with systemic malignancy, the weighted mean survival time was only 6.9 months [9].
In conclusion, numb chin syndrome can be caused by a variety of causes. Especially, although rare, it may appear as the first manifestation of systemic malignancies. In this case, the prognosis may be poor, so clinicians should never overlook the symptoms and, if necessary, perform thorough further investigation.
Notes
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Funding
None.
